Melatonin a léčba nespavosti
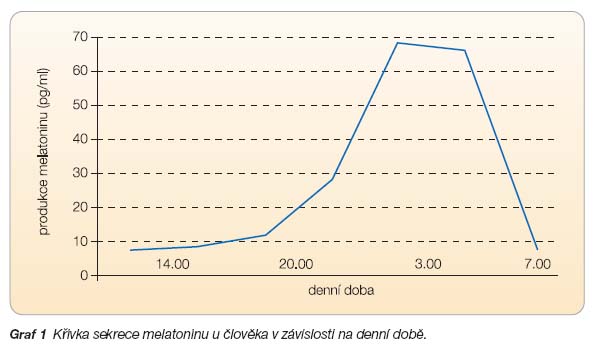
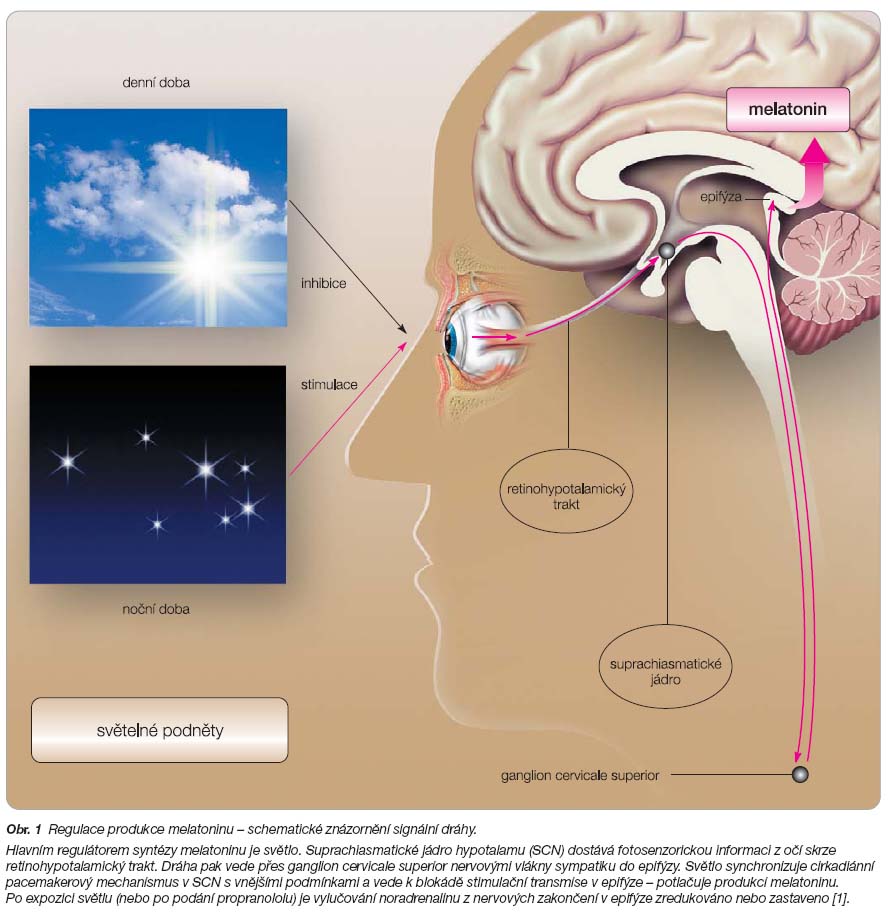
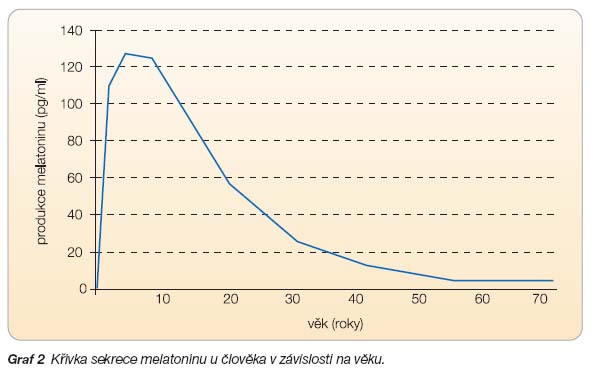
Melatonin, hormon produkovaný epifýzou v nočních hodinách, se u člověka uplatňuje jako časovač biologických rytmů a jako signál, který ohlašuje příchod spánku. Změněná úroveň sekrece a hladiny melatoninu byla zjištěna u různých psychiatrických poruch, jako je unipolární a bipolární deprese, sezonní afektivní porucha, bulimie, anorexie, panická porucha a obsedantně-kompulzivní porucha. Nízké hladiny melatoninu byly rovněž pozorovány u pacientů se schizofrenií. Se stoupajícím věkem produkce melatoninu klesá a zvyšuje se prevalence spánkových poruch, zejména nespavosti. V souvislosti s diagnostikou a terapií spánkových obtíží bývá jako dominující syndrom stále častěji popisován pocit nedostatečného osvěžení (vnímání nízké kvality spánku) a následně snížená aktivita ve dne. Melatonin může být užitečnou léčivou látkou v terapii poruch cirkadiánních rytmů, jako je syndrom změny časových pásem (jet-lag syndrome), zkracuje latenci usnutí a zároveň zlepšuje délku a kvalitu spánku. Melatonin může být rovněž využit jako krátkodobé hypnotikum u schizofrenních pacientů s nespavostí. Nízká produkce a sekrece melatoninu v noci byla prokázána u starších osob trpících nespavostí a jeho podávání se osvědčilo při léčbě spánkových obtíží u těchto pacientů. Ve srovnání s běžně předepisovanými látkami ze skupiny hypnotik, jako jsou benzodiazepiny a “Z” hypnotika (zolpidem, zopiklon), má melatonin několik klinicky významných předností, jednak nezpůsobuje ranní otupělost ani syndrom z odnětí, jednak není návykový.
Seznam použité literatury
- [1] Illnerová H, Borbély AA, Wirz-Justice A, Praško J. Circadian rhythmicity: from basic science to clinical approach. Clin Neurophysiol 2000; 53 (suppl): 339–347.
- [2] Sharma M, Palacios-Bois J, Schwartz G, et al. Circadian rhythms of melatonin and cortisol in aging. Biol Psychiatry 1989; 25: 305–319.
- [3] Lewy AJ, Ahmed S, Jackson JM, Sack RL. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992; 9: 380–392.
- [4] Dollins AB, Lynch HJ, Wurtman RJ, et al. Effect of pharmacological daytime doses of melatonin on human mood and performance. Psychopharmacology 1993; 112: 490–496.
- [5] Dahlitz M, Alvarez B, Vignau J, et al. Delayed sleep phase syndrome response to melatonin. Lancet 1991; 337: 1121–1124.
- [6] Tzischinsky O, Dagan Y, Lavie P. The effects of melatonin on the timing of sleep in patients with delayed sleep phase syndrome; in Touitou Y, Arendt J, Pevet P (eds): Melatonin and the Pineal Gland: From Basic Science to Clinical Application. Amsterdam, Excerpta Medica 1993; 351–354.
- [7] Dollins AB, Zhdanova IV, Wurtman RJ, et al. Effect of inducing nocturnal serum melatonin concentrations in daytime on sleep, mood, body temperature, and performance. Proc Natl Acad Sci USA 1994; 91: 1824–1828.
- [8] Ferrari E, Magri F, Locatelli M, et al. Chrono-neuroendocrine markers of the aging brain. Aging 1996; 8: 320–327.
- [9] Lushington K, Lack L, Dawson D. Melatonin production in good and poor elderly sleepers. Sleep 1995; 24A: 168.
- [10] Hajak G, Rodenbeck A, Staedt J, et al. Nocturnal plasma melatonin levels in patients with primary insomnia. J Pineal Res 1996; 19: 116–122.
- [11] Petterborg LJ, Thalen BE, Kjellman BF, Wetterberg L. Effect of melatonin replacement on serum hormone rhythms in a patient lacking endogenous melatonin. Brain Res Bull 1991; 27: 181–185.
- [12] Haimov I, Lavie P, Laudon M, et al. Melatonin replacement therapy of elderly insomniacs. Sleep 1995; 18: 598–603.
- [13] Garfinkel D, Laudon M, Nof D, Zisapel N. Improvement of sleep quality in elderly people by controlled release melatonin. Lancet 1995; 346: 541–544.
- [14] Garfinkel D, Laudon M, Zisapel N. Improvement of sleep quality by controlled-release melatonin in benzodiazepine-treated elderly insomniacs. Arch Gerontol Geriat 1997; 4: 223–231.
- [15] Wurtman RJ, Zhdanova I. Improvement of sleep quality by melatonin. Lancet 1995; 346: 1491.
- [16] Van den Heuvel C, Reid K, Dawson D. Effect of atenolol on nocturnal sleep and temperature in young men: reversal by pharmacological doses of melatonin. Psychol Behav 1997; 61: 795–802.
- [17] Hughes RJ, Sack R, Lewy A. The role of melatonin and circadian phase in age-related sleep-maintenance insomnia: assessment in a clinical trial of melatonin replacement. Sleep 1998; 21: 52–68.
- [18] Kripke D, Elliot J, Youngstedt S, Smith J. Melatonin: marvel or marker? Ann Med 1998; 30: 81–87.
- [19] Youngstedt SD, Kripke DF, Elliott JA. Melatonin excretion is not related to sleep in the elderly. J Pineal Res 1998; 24: 142–145.
- [20] Leger D, Laudon M, Zisapel N. Nocturnal 6-sulfatoxymelatonin excretion in insomnia and its relation to the response to melatonin replacement therapy. Am J Med 2004; 116: 91–95.
- [21] Wade AG, Ford I, Crawford G, et al. Efficacy of prolonged release melatonin in insomnia patients aged 55-80 years: quality of sleep and next-day alertness outcomes. Curr Med Res Opin 2007; 23: 2597–2605.
- [22] Lemoine P, Nir T, Laudon M, Zisapel N. Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. J Sleep Res 2007; 16: 372–380.
- [23] Srinivasan V, Spence DW, Pandi-Perumal SR, et al. Jet lag: Therapeutic use of melatonin and possible application of melatonin analogs. Travel Med Infect Dis 2008; 6: 17–28.
- [24] Arendt J, Aldhous M, Marks V. Alleviation of jet lag by melatonin: Preliminary results of controlled double blind trial. Br Med J 1986; 292: 1170.
- [25] Arendt J, Aldhous M. Further evaluation of the treatment of jet-lag by melatonin: A double-blind crossover study. Ann Rev Chronopharmacol 1988; 5: 53–55.
- [26] Petrie K, Conaglen JV, Thompson L, Chamberlain K. Effect of melatonin on jet lag after long haul flights. BMJ 1989; 298: 705–707.
- [27] Comperatore CA, Lieberman HR, Kirby AW, et al. Melatonin efficacy in aviation missions requiring rapid deployment and night operations. Aviat Space Environ Med 1996; 67: 520–524.
- [28] Paul AM, Gray G, Sardana TM, Pigeau RA. Melatonin and zopiclone as facilitators of early circadian sleep in operational air transport crews. Aviat Space and Environ Med 2004; 75: 439–443.
- [29] Garfinkel D, Zisapel N, Wainstein J, Laudon M. Facilitation of benzodiazepine discontinuation by melatonin. Arch Intern Med 1999; 159: 2456–2460.
- [30] Vissers FH, Knipschild PG, Crebolder HF. Is melatonin helpful in stopping the long-term use of hypnotics? A discontinuation trial. Pharm World Sci 2007; 29: 641–646.
- [31] Oldani A, Ferini-Strambi L, Zucconi M, et al. Melatonin and delayed sleep phase syndrome: Ambulatory polygraphic evaluation. Neuroreport 1994; 6: 132–134.
- [32] Palm L, Blennow G, Wetterberg L. Correction of non-24-hour sleep/wake cycle by melatoninin a blind retarded boy. Ann Neurol 1991; 29: 336–339.
- [33] Jan JE, Abroms IF, Freeman RD, et al. Rapid cycling in severely multidisabled children: A form of bipolar affective disorder? Pediatr Neurol 1994; 10: 34–39.
- [34] Jan JE, O Donnell ME. Use of melatonin in the treatment of paediatric sleep disorders. J Pineal Res 1996; 21: 193–199.
- [35] Dalton EJ, Rotendi D, Levitan RD, at al. Use of slow-release melatonin in treatment-resistant depression. J Psychiatry Neurosci 2000; 25: 48–52.
- [36] Andrade C, Srihari BS, Reddy KP, Chandramma L. Melatonin in medically ill patients with insomnia: a double-blind, placebo-controlled study. J Clin Psychiatry 2001; 62: 41–45.
- [37] Leppämäki S, Partonen T, Vakkuri O, et al. Effect of controlled-release melatonin on sleep quality, mood, and quality of life in subjects with seasonal or weather-associated changes in mood and behaviour. Eur Neuropsychopharmacol 2003; 13: 137–145.
- [38] Suresh Kumar PN, Andrade C, Bhakta SG, Singh NM. Melatonin in schizophrenic outpatients with insomnia: a double-blind, placebo-controlled study. J Clin Psychiatry 2007; 68: 237–241.
- [39] Van der Heijden KB, Smits MG, Van Someren EJ, et al. Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. J Am Acad Child Adolesc Psychiatry 2007; 46: 233–241.
- [40] Asayama K, Yamadera H, Ito T, et al. Double blind study of melatonin effects on the sleep-wake rhythm, cognitive and non-cognitive functions in Alzheimer type dementia. J Nippon Med Sch 2003; 70: 334–341.
- [41] Dowling GA, Burr RL, Van Someren EJ, et al. Melatonin and bright-light treatment for rest-activity disruption in institutionalized patients with Alzheimer s disease. J Am Geriatr Soc 2008; 56: 239–246.
- [42] Lam RW, Berkowitz AL, Berga SL, et al. Melatonin suppression in bipolar and unipolar mood disorders. Psychiatry Res 1990; 33: 129–134.
- [43] Souetre E, Salvati E, Belugou JL, et al. Circadian rhythms in depression and recovery: Evidence for blunted amplitude as the main chronobiological abnormality. Psychiatry Res 1989; 28: 263–278.
- [44] Kennedy SH, Garfinkel PE, Parienti V, et al. Changes in melatonin levels but not cortisol levels are associated with depression in patients with eating disorders. Arch Gen Psychiatry 1989; 46: 73–78.
- [45] Brismar K, Hylander B, Eliasson K, et al. Melatonin secretion related to side-effects of beta-blockers from the central nervous system. Acta Med Scand 1988; 223: 525–530.
- [46] Arendt J. Melatonin and the mammalian pineal gland. London, Chapman & Hall, 1995.